So you think your birth control is free now, thanks to the Affordable Care Act? Better double-check that with your insurance company.
In late July I received a letter from Blue Cross saying our coverage would change as of August 1st, including "Designated prescription contraception drugs." Hmm, "designated," I thought to myself. That sounds like a loophole. I better check it out. So I called Blue Cross to ask and they told me they wouldn't know until August 1st. So I said I would call back at that time, and called my mail-order pharmacy to ask them to hold any prescriptions that were pending until I called to approve them.
August 1st rolled around and I called Blue Cross again. The representative told me my specific oral contraceptive was covered. Yay, I thought.
My mail-order pharmacy robo-called to tell me I would be having an order filled on August 2nd, which I thought was odd, but hey, it would be free, so no harm no foul.
This morning I checked my bank account and my credit card had been charged. I called Prime and they told me that the information they had from Blue Cross said they would not be covering that type of birth control. They also said the order went through because somehow my doctor put in another prescription after I requested they not fill any prescriptions until I call, and somehow that superseded my request.
The pharmacy is refunding my money this one time.
I called Blue Cross to see what happened. This rep said the note in my file just said "advised on oral contraceptives" which is not useful. She told me that only certain types of oral contraceptives were covered at 100% under the ACA (as I'd suspected based on the wording) and that mine was not one of them. (Given that it is the generic for Ortho-Cyclen I find that pretty shocking.) I asked if there was a list of the covered birth control that could be found on their website or if she could email me one. She said no, she could read them to me over the phone. I asked how I would find out the information if it changes. She didn't have an answer for that so now not only do I have to switch birth control, I know I will now have to call in before every prescription refill to make sure that whatever I switch to is still covered.
She did make the lovely point that even the ones not covered at 100% would still be available at the standard prescription rate with my insurance. Apparently she hadn't looked at what kind of policy I have because I pay 100% of prescription drugs up through my deductible, which with my standard medications I will never hit in a year. I pointed that out and she said "oh." Because that is the only private insurance I could afford as a student and now as someone who is still seeking employment.
I also asked who sets the list of designated oral contraceptives. She said she could put me on hold to try to find out if I wanted. I said "please do." She did and came back and said the federal government set the list. I find that interesting and have no idea how to verify whether or not that is true.
Between the pharmacy and Blue Cross this took well over an hour on the phone. It is just good that I am damn persistent, by which I mean stubborn as a mule. But please do verify that your prescription is covered by your insurance before you order it again.
Here is the list I was given. If anyone else wants to call their health insurance company and see if they have a list and if the list matches up I would be very interested. Specifically to see if anything on this list is NOT on their list. Insurance companies can easily offer more (and would be wise to do so, in my opinion) but, if the list is truly mandated by federal law, could presumably not NOT include any of these.
- Camila
- Errin
- Heather
- Introvale
- Jolessa
- Jolivette
- Nora-BE
- Norethindrone
- Norgestimate/Ethinyl/ Estriadiol
- Quasense
- Trinessa
- Tri-previfem
- Tri-sprintec
(Interestingly these last two are generics for Ortho-tri-cyclen, which is like Ortho-cyclen [the one whose generics are not covered] except it includes a smaller amount of hormone in each succeeding week. I had been on this but my doctor switched me for medical reasons. Given that I don't think any of the ones above are anything like the one I'm on now, and I'm loathe to switch to something completely untried, I will probably have to switch back. Great.)
Dispatches from Nursing School
A journey through nursing school in Chicago.
Friday, August 3, 2012
Wednesday, March 2, 2011
Dreams and details - Week 7
The weeks have just flown by. We've had more clinical experience and our second exam. Clinicals are going well. My client last week had just been admitted that morning, which I learned was a bit of a different experience than all the clients I'd had before.
I can't talk much about clinicals, as of course I want to remain HIPAA compliant (besides just being ethical), but one thing I have really appreciated is that most clients are open to really sharing with us. They are dealing with so much just by virtue of being in the hospital and the fact that they are willing to talk to us, let us go through our assessments, and be so kind is really quite heartening.
I do have one story I can share. I was learning how to use the accucheck system last week and the nurse was showing me at the bedside. I was very hesitant about pushing it down because I didn't know how much pressure was needed or anything. The client gave a big yell of "OUCH!" and I jumped nearly a mile, at which point he started laughing and elbowing the nurse. Once I got over my panic and realized what had happened, I laughed a lot too. I also need to remember to never tell my uncles that story, for fear they will do the same thing if anyone ever has to check their blood glucose levels.
I did finally get it, by the way. Heh.
In skill lab we've learned how to put on sterile gloves and set up a sterile field, change IV fluids and set up piggybacks, and how to insert and take out an NG tube. This mannequin looks surprised about his NG tube. I don't know why, because I thoroughly explained the procedure before I inserted it:
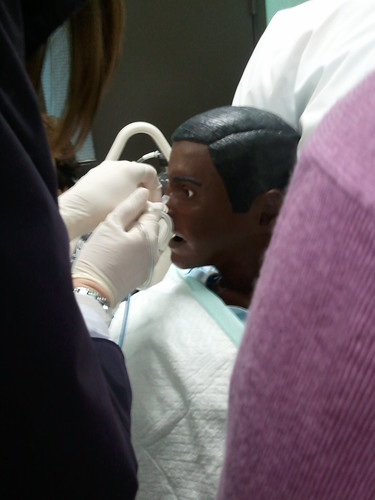
(That is someone else about to take it out.)
And this is our IV arm:

In class we are moving along quickly, after having had one day of lecture stolen from us by the blizzard. This last exam included pneumonia, peptic ulcer disease, cholecystitis, and inflammation. We covered UTIs today and started fluids and electrolytes, which promises to be a long but interesting chapter. I'm now glad about how much my anatomy & physiology professor stressed learning things like ADH, because it all started coming back during the lecture today.
Microbiology is still quite enjoyable; we did a Kirby-Bauer lab and some differential staining, which was fun. We also did an antiseptic-disinfectant lab where we were all supposed to bring cleaning products and we tested how well they worked. I brought in a free bottle of a pet-mess cleaning product I'd gotten with some kitty litter and much to my surprise, it actually did work. (Urinal cakes did not. I did not bring that.)
And on the topic of "nursing has taken over my braaaain," last night I dreamt I was at a hospital for clinicals and my patient started crashing. The nurse told me to "call a code" so I ran out of the room then realized I DIDN'T KNOW HOW TO CALL A CODE. "We haven't covered that yet!" I thought, as I looked around, and in the dream realized that instead of a hospital hallway full of medical staff who could help, the hallway was like a clinic waiting room. I didn't feel like I should start yelling so I said "code?" and wandered around looking for a doctor. Finally I found one and we eventually made it back to the room and out came a surgeon covered in blood, wearing an animal-butcher apron, and I went in and the room was full of more people also covered in blood. I woke up trying to find the patient to see if he was alive or dead.
I am sure this dream says many things, about anxiety and stress and not feeling quite prepared, but I think mostly it says to stop watching House before bed, especially on the night after clinicals.
I can't talk much about clinicals, as of course I want to remain HIPAA compliant (besides just being ethical), but one thing I have really appreciated is that most clients are open to really sharing with us. They are dealing with so much just by virtue of being in the hospital and the fact that they are willing to talk to us, let us go through our assessments, and be so kind is really quite heartening.
I do have one story I can share. I was learning how to use the accucheck system last week and the nurse was showing me at the bedside. I was very hesitant about pushing it down because I didn't know how much pressure was needed or anything. The client gave a big yell of "OUCH!" and I jumped nearly a mile, at which point he started laughing and elbowing the nurse. Once I got over my panic and realized what had happened, I laughed a lot too. I also need to remember to never tell my uncles that story, for fear they will do the same thing if anyone ever has to check their blood glucose levels.
I did finally get it, by the way. Heh.
In skill lab we've learned how to put on sterile gloves and set up a sterile field, change IV fluids and set up piggybacks, and how to insert and take out an NG tube. This mannequin looks surprised about his NG tube. I don't know why, because I thoroughly explained the procedure before I inserted it:
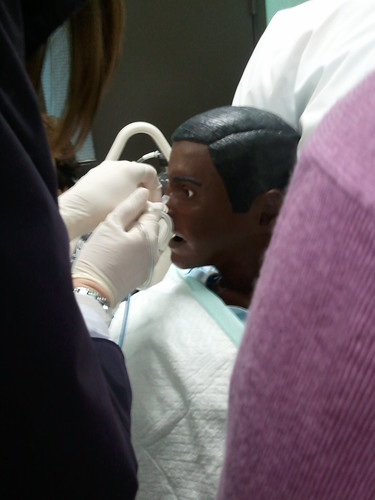
(That is someone else about to take it out.)
And this is our IV arm:

In class we are moving along quickly, after having had one day of lecture stolen from us by the blizzard. This last exam included pneumonia, peptic ulcer disease, cholecystitis, and inflammation. We covered UTIs today and started fluids and electrolytes, which promises to be a long but interesting chapter. I'm now glad about how much my anatomy & physiology professor stressed learning things like ADH, because it all started coming back during the lecture today.
Microbiology is still quite enjoyable; we did a Kirby-Bauer lab and some differential staining, which was fun. We also did an antiseptic-disinfectant lab where we were all supposed to bring cleaning products and we tested how well they worked. I brought in a free bottle of a pet-mess cleaning product I'd gotten with some kitty litter and much to my surprise, it actually did work. (Urinal cakes did not. I did not bring that.)
And on the topic of "nursing has taken over my braaaain," last night I dreamt I was at a hospital for clinicals and my patient started crashing. The nurse told me to "call a code" so I ran out of the room then realized I DIDN'T KNOW HOW TO CALL A CODE. "We haven't covered that yet!" I thought, as I looked around, and in the dream realized that instead of a hospital hallway full of medical staff who could help, the hallway was like a clinic waiting room. I didn't feel like I should start yelling so I said "code?" and wandered around looking for a doctor. Finally I found one and we eventually made it back to the room and out came a surgeon covered in blood, wearing an animal-butcher apron, and I went in and the room was full of more people also covered in blood. I woke up trying to find the patient to see if he was alive or dead.
I am sure this dream says many things, about anxiety and stress and not feeling quite prepared, but I think mostly it says to stop watching House before bed, especially on the night after clinicals.
Thursday, February 10, 2011
First injection, first exam - Week 4
Well, I made it through another week. It was a big one!
Tuesday we had clinicals and, since I had my OR trip last week, it was my first week this semester with a patient. I'm at the same hospital as last semester but on a new floor, and it was my first taste of how different each hospital floor can really be. I'd become accustomed to the floor we were on last semester and this one was a lot quieter, I'd say - but we'll see if I feel the same way after a few more weeks.
Of course I can't talk about my client, but I can say that I gave my first injection! It was a subcutaneous heparin injection. My instructor was there supervising, of course, and started quizzing me. "Do you aspirate a subq injection?" "No." "Do you massage after giving a subq injection?" "No." At this point the client joined in: "why not?" He didn't say this in a challenging way; rather, I'm pretty sure he knew the answer and just wanted to be part of the quizzing process. I was a bit flustered and answered something like "because it's a subq injection" (which, let's be fair, is of course how I memorized it for the test), but my prof came back with "come on, why wouldn't you massage a heparin injection?" at which point I had gathered my wits a bit and was able to reply "because it's a blood thinner and you could damage the tissue." Prof and client both satisfied, I gave the injection. It was a success! He even said it didn't hurt. And I don't think he would have said that just to make me feel good (although you never know).
Once everything was taken care of and we left the room to document, I actually did a bit of a bounce. I gave my first injection! It was really exciting for me. I was so apprehensive to begin with, just because it seemed so serious - sticking a needle in someone is not a small matter - but I did it and it was ok and he was fine and everything worked out. I feel like it's areal milestone of some sort. Hurrah!
We also had our first exam this week. I was quite apprehensive (new professor, new exam style!) but it turns out I got a 49/50, so I'm pretty happy. Hoo-rah! And that is after my cell phone/alarm clock turned off overnight before the exam and I woke up 5 minutes before I had planned to leave the house. (That is NOT a good way to start an exam morning. Let me tell you what. The level of adrenaline I had rushing through my body was intense. It was, however, a good review of the stages of stress that were on the exam.)
Tuesday we had clinicals and, since I had my OR trip last week, it was my first week this semester with a patient. I'm at the same hospital as last semester but on a new floor, and it was my first taste of how different each hospital floor can really be. I'd become accustomed to the floor we were on last semester and this one was a lot quieter, I'd say - but we'll see if I feel the same way after a few more weeks.
Of course I can't talk about my client, but I can say that I gave my first injection! It was a subcutaneous heparin injection. My instructor was there supervising, of course, and started quizzing me. "Do you aspirate a subq injection?" "No." "Do you massage after giving a subq injection?" "No." At this point the client joined in: "why not?" He didn't say this in a challenging way; rather, I'm pretty sure he knew the answer and just wanted to be part of the quizzing process. I was a bit flustered and answered something like "because it's a subq injection" (which, let's be fair, is of course how I memorized it for the test), but my prof came back with "come on, why wouldn't you massage a heparin injection?" at which point I had gathered my wits a bit and was able to reply "because it's a blood thinner and you could damage the tissue." Prof and client both satisfied, I gave the injection. It was a success! He even said it didn't hurt. And I don't think he would have said that just to make me feel good (although you never know).
Once everything was taken care of and we left the room to document, I actually did a bit of a bounce. I gave my first injection! It was really exciting for me. I was so apprehensive to begin with, just because it seemed so serious - sticking a needle in someone is not a small matter - but I did it and it was ok and he was fine and everything worked out. I feel like it's areal milestone of some sort. Hurrah!
We also had our first exam this week. I was quite apprehensive (new professor, new exam style!) but it turns out I got a 49/50, so I'm pretty happy. Hoo-rah! And that is after my cell phone/alarm clock turned off overnight before the exam and I woke up 5 minutes before I had planned to leave the house. (That is NOT a good way to start an exam morning. Let me tell you what. The level of adrenaline I had rushing through my body was intense. It was, however, a good review of the stages of stress that were on the exam.)
Tuesday, February 1, 2011
Second Semester - Week Three (the OR visit!)
We've completed our third week of nursing school! On a Tuesday night, you might ask? That's a bit quick on the draw. Well, see, we have this thing in Chicago right now called a "blizzard" so school was canceled from today at 2PM all through tomorrow. I'll still have microbiology on Thursday, but that's not nursing class, so I consider it a true statement.
The snow is not without it's drama - oh believe you me, it is not. I have Tuesday morning clinicals and I was on tenterhooks, hoping with all my might it wouldn't be canceled. I realize it sounds slightly overzealous to be that eager for clinicals, but that's because today was my day to observe an OR procedure. Due to the OR schedule not everyone in our group would be able to observe one, and I managed to draw a lucky piece of paper. The idea that I'd lose out on my one chance due to weather was so appalling that it actually kept me up the night before. Luckily the roads were clear until well after our clinicals were over, so we were all set to go.
The procedure for OR observation is that we meet the person from the OR in the lobby at 7:30, and they bring us to the rooms. (Technically the first thing is that they tell you to make sure you eat breakfast - it helps keep people from feeling sick, apparently.) I was observing as well as another student from a different instructor's group, so we met in the lobby and stood around awkwardly for a while waiting for our contact. Once she arrived we hit our first roadblock - lots of surgeries had been canceled due to the impending blizzard, so she wasn't sure what kind of surgery we'd be able to see.
We got to the OR area and our contact brought us to our locker rooms and instructed us to change into our disposable clean outfits, grab a head covering (called a bonnet, not a "hair mask" which is what I came up with before I learned the proper term), and meet her on the other side of the locker room. I got dressed and as they only had mediums, I had to tuck my shirt in and tie my pants incredibly tightly. I am not size medium, as you can see.

Once we were suitably dressed (shoe covers were provided on the other side, as it were), we proceeded to the OR room. We put on our masks and went in. The client was already anesthetized and they were prepping him. This included putting foam all around him for stability, taping the foam all up, putting his legs in boots that were actually SCDs (to prevent deep vein thrombosis), putting blankets and a specific actual warming machine on him, and then covering all parts of him except the part being operated on. Really nothing is visible at all, and clearly that is safest for the patient but it was strange to watch happen. Like a magician and a disappearing act. It was fascinating (and I might use that word a lot, here) to watch the transition - the team worked together so well, and knew exactly what they were doing, all these procedures and processes that seemed arcane and confusing to me. Everyone had a role and was busy so I definitely didn't want to interrupt to ask questions at this point, although we did have chances to later.
Also during the setup, I noticed some tubing (I think for suction but I'm not positive) coiled on the floor and was concerned that it might be a trip hazard. As someone coming from a computer and technology background, those are the sorts of things I'm primed to notice - and lots of time I'm the only one who does. In this case, though, almost as soon as I noticed, the anesthetist put a towel over them, flattening them out and making it safe. That impressed me.
Once the client was ready, the robot was pushed into place. The procedure we were viewing was a robotic prostatectomy, so the first thing was making the incisions for the robot arms, camera, lights, etc. Based on what I've been told I assume this is when most people feel faint or sick, and I had been curious to know if I'd have that sort of reaction, but I didn't. We'd been given instructions on what to do if we felt like we were going to faint (go stand against the far wall so if you do, you fall safely and no one has to break sterility), but I know I never felt close and I don't think the other student did either.
Once the robot was ready, one of the surgeons went to the controls (which looked like a big virtual-reality console as imagined 20 years ago) and the other surgeon stood with the client. The scrub nurse was assisting as requested and needed, maintaining sterility, but she also did a fantastic job of answering our questions and making sure we could see the monitors. We had two different circulating nurses at different times, and they also did a great job of answering our questions as well. I didn't get to talk to the anesthetist, unfortunately. But just watching how the team worked together was great.
Watching the surgeons and scrub nurse in action was so interesting. Sterile fields are something we see on TV and in movies, with surgeons being gowned and gloved and people walking around with their hands above their waists, but it's just a bit more real to see it in person. I was quite interested and impressed by how it seemed so natural to all of them. The nurse was quite good at manipulating the environment without using her hands (she was a pro at moving the stool with her feet). I was also quite interested to see how they all had sterile ways of doing other things - there was a towel she could use to move a monitor, for instance, and they had handles to attach to the lights so that the sterile people could still move them. Certain pieces of machinery (for instance the carbon dioxide machine) had plastic over the front of it, so the surgeons and scrub nurse were the ones manipulating that, but things like the sterile water for irrigation and the suction tubing didn't, so the circulating nurse was responsible for that. I wondered if they set up practice rooms for new scrub nurses and for new medical students, so you can practice sterile procedure and someone, I don't know, presses a buzzer whenever you do something that would contaminate you.
The client was having his pelvic lymph nodes removed as well as his prostate, so the surgeons removed the lymph nodes first. Lymph nodes are kind of sticky, it seemed like. Watching the robot journey through the body was amazing. It was like the Magic Schoolbus, but with more robot arms and blood. We hadn't really had a briefing on what all the robotic instruments did, but I was able to figure it out. There was one just for grabbing, one for more dexterous grabbing (which was also later used for suturing - suturing! with tiny robot hands!), one that cauterized, one that irrigated, one for suction, and scissors (which, I learned later, also cauterized). The combined effect of the irrigation and the cauterization? Made it look like there was weather in the body - it looked like mist, or fog, blowing around in the body cavity. Brilliant. I also learned that they inflate the body cavity with carbon dioxide, to give more working room. The surgeons would request different levels of inflation at various points, based on what was happening at the time. Which was also really interesting to me.
One thing I found out is that the robotic prostatectomy is much safer than the open prostatectomy - not only for the normal reasons of lesser chance of infection and quicker recovery time, but because the nerves controlling sexual function and urinary function are attached to the prostate area. During open prostatectomies these are often severed, even though the surgeons do their best not to, just due to the greater size of the instruments and less level of available detail. The robotic procedure, on the other hand, actually peels the nerves away from the prostate, which gives a much greater chance for leaving the nerves intact. A thoroughly convincing benefit, I'm sure everyone will agree.
The procedure took about 3 hours and it was amazing how much was accomplished with minimal disruption to the body. I think the weirdest part was seeing the actual removed items come out - they put the items in a little bag, which closes, and then gets pulled out. I asked if anyone ever asked to keep anything that's removed but I was told that the specimens get sent to pathology for testing. When the prostate was removed, we actually got to put gloves on and hold it and see if we could feel the cancer. (I don't really know what prostates are supposed to feel like, so the answer was no, I couldn't tell where the cancer was.)
Once the client was waking up we got to see the anesthetist in action. She asked the client to wiggle his toes, open his mouth, and then put an oxygen mask on him. His oxygen levels were a bit low so she kept having to ask him to take some deep breaths until it went back to normal, but that happened quickly so it really went quite smoothly. The client was understandably groggy and was quickly transferred onto a bed to bring him to the recovery room. I felt very lucky in that one of the nurses asked me to help with the transfer from OR table to bed! I helped! It was a great feeling, very triumphant.
After that we talked a little more with the nurses and surgeons, and made sure we had all the information we needed to write our reports for class. Everyone was great and I feel so incredibly lucky that I got to have this experience. I am now wondering if I want to be an OR nurse, and that's saying something. It was definitely one of the more interesting experiences of my life.
In other news, the blizzard is in full force outside and I actually heard some of the hospital staff talking about the preparations they were making, which is funny since I then read about the same preparations here. I am safe inside with my studying and actually have already finished some homework and studying, and while there is plenty more to be done I feel confident I'll be ready in time for our exam (which was scheduled for next Monday, but due to classes being canceled tomorrow, will now be on Wednesday). I should probably write my microbiology lab report first thing in the morning, though.
Goodnight, all. I'm going to fall asleep listening to the thundersnow. (Thundersnow! An operation! What a day!)
The snow is not without it's drama - oh believe you me, it is not. I have Tuesday morning clinicals and I was on tenterhooks, hoping with all my might it wouldn't be canceled. I realize it sounds slightly overzealous to be that eager for clinicals, but that's because today was my day to observe an OR procedure. Due to the OR schedule not everyone in our group would be able to observe one, and I managed to draw a lucky piece of paper. The idea that I'd lose out on my one chance due to weather was so appalling that it actually kept me up the night before. Luckily the roads were clear until well after our clinicals were over, so we were all set to go.
The procedure for OR observation is that we meet the person from the OR in the lobby at 7:30, and they bring us to the rooms. (Technically the first thing is that they tell you to make sure you eat breakfast - it helps keep people from feeling sick, apparently.) I was observing as well as another student from a different instructor's group, so we met in the lobby and stood around awkwardly for a while waiting for our contact. Once she arrived we hit our first roadblock - lots of surgeries had been canceled due to the impending blizzard, so she wasn't sure what kind of surgery we'd be able to see.
We got to the OR area and our contact brought us to our locker rooms and instructed us to change into our disposable clean outfits, grab a head covering (called a bonnet, not a "hair mask" which is what I came up with before I learned the proper term), and meet her on the other side of the locker room. I got dressed and as they only had mediums, I had to tuck my shirt in and tie my pants incredibly tightly. I am not size medium, as you can see.

Once we were suitably dressed (shoe covers were provided on the other side, as it were), we proceeded to the OR room. We put on our masks and went in. The client was already anesthetized and they were prepping him. This included putting foam all around him for stability, taping the foam all up, putting his legs in boots that were actually SCDs (to prevent deep vein thrombosis), putting blankets and a specific actual warming machine on him, and then covering all parts of him except the part being operated on. Really nothing is visible at all, and clearly that is safest for the patient but it was strange to watch happen. Like a magician and a disappearing act. It was fascinating (and I might use that word a lot, here) to watch the transition - the team worked together so well, and knew exactly what they were doing, all these procedures and processes that seemed arcane and confusing to me. Everyone had a role and was busy so I definitely didn't want to interrupt to ask questions at this point, although we did have chances to later.
Also during the setup, I noticed some tubing (I think for suction but I'm not positive) coiled on the floor and was concerned that it might be a trip hazard. As someone coming from a computer and technology background, those are the sorts of things I'm primed to notice - and lots of time I'm the only one who does. In this case, though, almost as soon as I noticed, the anesthetist put a towel over them, flattening them out and making it safe. That impressed me.
Once the client was ready, the robot was pushed into place. The procedure we were viewing was a robotic prostatectomy, so the first thing was making the incisions for the robot arms, camera, lights, etc. Based on what I've been told I assume this is when most people feel faint or sick, and I had been curious to know if I'd have that sort of reaction, but I didn't. We'd been given instructions on what to do if we felt like we were going to faint (go stand against the far wall so if you do, you fall safely and no one has to break sterility), but I know I never felt close and I don't think the other student did either.
Once the robot was ready, one of the surgeons went to the controls (which looked like a big virtual-reality console as imagined 20 years ago) and the other surgeon stood with the client. The scrub nurse was assisting as requested and needed, maintaining sterility, but she also did a fantastic job of answering our questions and making sure we could see the monitors. We had two different circulating nurses at different times, and they also did a great job of answering our questions as well. I didn't get to talk to the anesthetist, unfortunately. But just watching how the team worked together was great.
Watching the surgeons and scrub nurse in action was so interesting. Sterile fields are something we see on TV and in movies, with surgeons being gowned and gloved and people walking around with their hands above their waists, but it's just a bit more real to see it in person. I was quite interested and impressed by how it seemed so natural to all of them. The nurse was quite good at manipulating the environment without using her hands (she was a pro at moving the stool with her feet). I was also quite interested to see how they all had sterile ways of doing other things - there was a towel she could use to move a monitor, for instance, and they had handles to attach to the lights so that the sterile people could still move them. Certain pieces of machinery (for instance the carbon dioxide machine) had plastic over the front of it, so the surgeons and scrub nurse were the ones manipulating that, but things like the sterile water for irrigation and the suction tubing didn't, so the circulating nurse was responsible for that. I wondered if they set up practice rooms for new scrub nurses and for new medical students, so you can practice sterile procedure and someone, I don't know, presses a buzzer whenever you do something that would contaminate you.
The client was having his pelvic lymph nodes removed as well as his prostate, so the surgeons removed the lymph nodes first. Lymph nodes are kind of sticky, it seemed like. Watching the robot journey through the body was amazing. It was like the Magic Schoolbus, but with more robot arms and blood. We hadn't really had a briefing on what all the robotic instruments did, but I was able to figure it out. There was one just for grabbing, one for more dexterous grabbing (which was also later used for suturing - suturing! with tiny robot hands!), one that cauterized, one that irrigated, one for suction, and scissors (which, I learned later, also cauterized). The combined effect of the irrigation and the cauterization? Made it look like there was weather in the body - it looked like mist, or fog, blowing around in the body cavity. Brilliant. I also learned that they inflate the body cavity with carbon dioxide, to give more working room. The surgeons would request different levels of inflation at various points, based on what was happening at the time. Which was also really interesting to me.
One thing I found out is that the robotic prostatectomy is much safer than the open prostatectomy - not only for the normal reasons of lesser chance of infection and quicker recovery time, but because the nerves controlling sexual function and urinary function are attached to the prostate area. During open prostatectomies these are often severed, even though the surgeons do their best not to, just due to the greater size of the instruments and less level of available detail. The robotic procedure, on the other hand, actually peels the nerves away from the prostate, which gives a much greater chance for leaving the nerves intact. A thoroughly convincing benefit, I'm sure everyone will agree.
The procedure took about 3 hours and it was amazing how much was accomplished with minimal disruption to the body. I think the weirdest part was seeing the actual removed items come out - they put the items in a little bag, which closes, and then gets pulled out. I asked if anyone ever asked to keep anything that's removed but I was told that the specimens get sent to pathology for testing. When the prostate was removed, we actually got to put gloves on and hold it and see if we could feel the cancer. (I don't really know what prostates are supposed to feel like, so the answer was no, I couldn't tell where the cancer was.)
Once the client was waking up we got to see the anesthetist in action. She asked the client to wiggle his toes, open his mouth, and then put an oxygen mask on him. His oxygen levels were a bit low so she kept having to ask him to take some deep breaths until it went back to normal, but that happened quickly so it really went quite smoothly. The client was understandably groggy and was quickly transferred onto a bed to bring him to the recovery room. I felt very lucky in that one of the nurses asked me to help with the transfer from OR table to bed! I helped! It was a great feeling, very triumphant.
After that we talked a little more with the nurses and surgeons, and made sure we had all the information we needed to write our reports for class. Everyone was great and I feel so incredibly lucky that I got to have this experience. I am now wondering if I want to be an OR nurse, and that's saying something. It was definitely one of the more interesting experiences of my life.
In other news, the blizzard is in full force outside and I actually heard some of the hospital staff talking about the preparations they were making, which is funny since I then read about the same preparations here. I am safe inside with my studying and actually have already finished some homework and studying, and while there is plenty more to be done I feel confident I'll be ready in time for our exam (which was scheduled for next Monday, but due to classes being canceled tomorrow, will now be on Wednesday). I should probably write my microbiology lab report first thing in the morning, though.
Goodnight, all. I'm going to fall asleep listening to the thundersnow. (Thundersnow! An operation! What a day!)
Friday, January 21, 2011
Second Semester - Week One
This week was our first week of school, and even though we started on Tuesday instead of Monday I feel like it counted for a whole week. This semester I'm taking both Nursing 102 and microbiology, so it's going to be a bit busier than last semester.
The first day of school was a clinical day, but we weren't in the hospital yet. We were on campus and had 6 hours of lecture/administrative work, as well as a nursing critical-thinking exam. That was a bit confusing, I think, because we were told ahead of time that we'd have this exam but not why, or if it counted towards our grade, or what it was all about. It turned out it was a metric for the school, not for our grades, so after that I didn't really worry about it. Which served me well, since I got a 920/1000. I have no idea what a good score is but that sounds high so I'll take it.
I have a different instructor for my nursing class this semester, so I am also getting to know her style as well as a whole new set of classmates - only one of my classmates from the first semester is in my class, and he won't be in my clinical group. As always it's interesting to get to know a whole new group of personalities and see where we mesh and where we divide.
We had our first skill lab, too, and started learning to give injections! They are not starting us slowly, that's for sure. We managed to cover intramuscular and intradermal injections but didn't have time to cover subcutaneous, so we will cover that next week. We had real needles and dummy body parts on which to practice. It was quite exciting. Here's a picture from skill lab:

My microbiology class is proving interesting already - we've already had a lab and been assigned our microscopes to use throughout the semester. Mine seems good, which is a relief, and I like that we'll keep the same one so we get to know the instrument. Everyone told me that this professor really teaches you to use a microscope properly, so I'm hoping that in this class I'll finally learn how to not get headaches when I look through one for more than half an hour. I really enjoy microscopy and the nerdier aspects of science, so getting my brain on board with that would be nice. Plus, microbiology really is interesting, as a topic.
On the whole, while I'm anxious about the amount of time I'll need to study this semester, and the workload, I'm still excited and ready to go.
The first day of school was a clinical day, but we weren't in the hospital yet. We were on campus and had 6 hours of lecture/administrative work, as well as a nursing critical-thinking exam. That was a bit confusing, I think, because we were told ahead of time that we'd have this exam but not why, or if it counted towards our grade, or what it was all about. It turned out it was a metric for the school, not for our grades, so after that I didn't really worry about it. Which served me well, since I got a 920/1000. I have no idea what a good score is but that sounds high so I'll take it.
I have a different instructor for my nursing class this semester, so I am also getting to know her style as well as a whole new set of classmates - only one of my classmates from the first semester is in my class, and he won't be in my clinical group. As always it's interesting to get to know a whole new group of personalities and see where we mesh and where we divide.
We had our first skill lab, too, and started learning to give injections! They are not starting us slowly, that's for sure. We managed to cover intramuscular and intradermal injections but didn't have time to cover subcutaneous, so we will cover that next week. We had real needles and dummy body parts on which to practice. It was quite exciting. Here's a picture from skill lab:

My microbiology class is proving interesting already - we've already had a lab and been assigned our microscopes to use throughout the semester. Mine seems good, which is a relief, and I like that we'll keep the same one so we get to know the instrument. Everyone told me that this professor really teaches you to use a microscope properly, so I'm hoping that in this class I'll finally learn how to not get headaches when I look through one for more than half an hour. I really enjoy microscopy and the nerdier aspects of science, so getting my brain on board with that would be nice. Plus, microbiology really is interesting, as a topic.
On the whole, while I'm anxious about the amount of time I'll need to study this semester, and the workload, I'm still excited and ready to go.
Friday, January 7, 2011
Winter break - update on the end of first semester
I realize I haven't written in a while and one of my goals for the New Year is to do better, so I'm hoping to start off right! We had finals in early/mid-December (is it bragging to mention that I did get an A, and did well in my clinical evaluations?) and have been on break since, and I will say I have needed the time to recover and get ready for the next semester. We start the day after MLK day, so just over a week now. I am looking forward to it but besides Nursing 102 I'll also be taking microbiology, so that is definitely going to keep me busy.
We signed up for a new clinical rotation but I ended up at the same hospital, so I'll be back at the University of Chicago. I would like to have opportunities in other hospitals to get a wider variety of experience, but I also liked U of C so I think it'll be ok. The other difference is that this is a 6:30AM - 12:30PM slot, instead of 7AM - 1PM, so I'm going to have to wake up even earlier on Tuesdays! (The benefit to this? Minimal traffic on the way there. It's kind of fun to drive on the Chicago roads that early in the morning.)
One of the most interesting things we did at the end of last semester was work with the Medi-man that's located in the school. The Medi-man looks like a mannequin, but is hooked up to a computer system and has quite complex internal workings. The Medi-man breathes, has a pulse and blood pressure, can pass bodily fluids, has pupils that contract and dilate, and even responds to things like pills you put in the mouth, oxygen, and the AED. They can run different scenarios on the patient so that students can practice responding in an emergency without, you know, having to worry about killing an actual person. Or waiting around for the right emergency to happen. While we were in there they had him crash and two of the students had to do CPR to revive him - and it worked! (Our professor told us she had the person who runs the lab set it so the Medi-man wouldn't "die" for the first-years, because it can be too emotionally upsetting.)
Anyway as I'm sure you can imagine I found this utterly fascinating and asked if we could see the controls. There's actually a two-way mirror into the room so the person who runs the lab can watch from the control room, so we went back there and saw the computer and systems that run it. The software is pretty interesting - the whole system is set up so like in real life you can't just change one variable; if you change the patient's oxygen levels that affects other things, and the software figures it out for you. The lab manager said that when they first acquired the system they had to build their own scenarios for each simulation they wanted to do, but now there are also off-the-shelf ones you can buy from the company (I couldn't believe they didn't do that right away - it seemed like such a logical money-making opportunity). The Medi-man also has things like room gas sensors so it knows how to respond to the oxygen, and there are actually big tanks of oxygen and other gases in the back hooked up to the Medi-man so it can behave properly. We also saw the servers where all this is stored. (My IT security training kicked in and I started wondering why it wasn't locked up more than it is but I refrained from mentioning it.)
So that is a whole side of HIT that I never even thought of before I experienced it, but right away I realized what a valuable tool it was. I can't wait until we get to do more simulations in our second semester!
Monday, November 1, 2010
Just past midterms, first semester
Nursing school has proceeded apace. A couple weeks ago was midterm, today we have our third exam, and things just keep moving along. I can't believe it, but that means we're over 1/8 done.
Here are some notes from along the way:
Here are some notes from along the way:
- We've actually started doing vital signs and, as of this week, passing meds! This was my first week of officially doing both on our clinical site and I realized I was slightly intimidated when I put the vital signs I Actually Took Myself into my patient's computer chart. It somehow made things way more official than they had been up until that moment! I also gave my first medication, after of course I triple-checked it and so did my instructor. It was Coreg, an anti-hypertensive, and I am guessing I will probably never forget it.
- I have also been practicing taking blood pressure on practically everyone I know. Luckily all of my friends and family have been pretty patient with this.
- I really can't imagine what the hospitals were like before the EMRs! I know, I know, everyone is going to call me a young whippersnapper but from a safety perspective, the level of error-checking is great. My instructor has told us about hospitals that have even more advanced systems than U of C, especially with regards to medication and preventing medication errors, and honestly they all seem like such good ideas that I wish all hospitals had them all. I especially like the one where you have to scan the person and the med before you give the med and it warns you if it's the wrong one. I truly wish all hospitals had that. Even the best doctor and nurse can make a human error, because no one is ever perfect, and having safeguards is never a bad thing.
- And oh! Our teacher held up a big magazine article about Dennis Quaid when we first started talking about meds. I got very excited and of course had to explain that he'd spoken at my former employer's annual conference.
- Our instructors have all made a big deal about starting study groups, but I tried to attend one and have found that it just doesn't match my style. I like discussing philosophies and hypothetical examples with my classmates, but when it actually comes to learning the material, I work much better alone. At first I wondered if I was doing things wrong, but I remembered that I've always been this way, so I decided not to worry about it any further.
- We've had our first two exams, and while my stress levels have gone through the roof I managed to get As on both. We also had our midterm clinical evaluations, which included some good feedback and that I am doing well on the skills-level but also included my clinical instructor asking if I was sure I wanted to be a nurse and telling me I could only answer that by looking into my own heart! It turns out she and I have very different styles so she interpreted my learning-mode-behavior as hesitancy and uncertainty. But I think we got it straightened out. As I'm sure you can imagine it was a rather alarming few minutes, though.
Really it's amazing. I know I have so much left to learn, and I feel like I have learned very little when I think about actually taking care of patients, but when I look back to my first week of classes it seems like a lifetime ago in terms of how far I've come. There's just so much to learn and so much change happening so quickly!
Subscribe to:
Posts (Atom)